Learn About
Continuous Glucose Monitor (CGM) Placement and Insulin Pump Therapy
Our team of physicians are board certified physicians by the American Board of Internal Medicine and have been practicing Endocrinology with an emphasis in diabetes, non-surgical weight loss and Thyroid disease. Below are the services that we provide. Please call our office 786-433-2450 if you have any questions or would like to schedule an appointment.


Learn About
Insulin Pump Therapy
Our team of physicians are board certified physicians by the American Board of Internal Medicine and have been practicing Endocrinology with an emphasis in diabetes, non-surgical weight loss and Thyroid disease. Below are the services that we provide. Please call our office 786-433-2450 if you have any questions or would like to schedule an appointment.
An insulin pump is a small device that is a convenient method for insulin delivery for people with diabetes, replacing the conventional, multiple, daily insulin injections. Insulin pump therapy allows you to set a basal rate, or background insulin, that is delivered continuously throughout the day and night to support normal body function. The insulin pump delivers insulin through a small tube which is attached to an even smaller cannula (tube). The cannula is inserted under the skin by a small needle every 2 to 3 days. The pump has an insulin reservoir. This reservoir must be filled with insulin by the patient every 2 to 3 days when the cannula is replaced.
Appropriate candidates for the insulin pump include diabetics who:
- Diabetics type 1 and type 2
- Self-monitor and record blood glucose levels at least six times daily
- Treat low blood glucose levels appropriately
- Demonstrate ability to operate the pump
At Miami Diabetes and Endocrinology with strongly believe that education is essential. Our physicians are Certified Insulin Pump Trainers. During consultation, together will review your current diabetes care plan and identify if and which pump would work best for you. Over the course of several visits, we will educate and review with you about maintaining the pump, pump replacement, insulin administration and technology needed to monitor and optimize your glucose levels.
In people without diabetes, pancreatic cells called “islet cells” detect glucose in the blood and release insulin or glycogen to keep the glucose level in a safe range.
Up until a few year ago, insulin pumps were administering insulin every hour (also known as basal or background rate) and patients would do a “meal bolus” (patient-administered insulin dose). This required:
- an insulin pen (for insulin delivery) for the “meal bolus”.
- a blood glucose monitor or a CGM (for glucose level assessment).
- our “brains” to calculate the dose required for the “meal bolus” and our “fingers” to deliver it to complete the loop.
“Closing the loop” means making it happen automatically. This means the pump has a calculator or algorithm replace our brains and fingers. The algorithm adjusts the basal (background) insulin every few minutes as necessary, to keep the glucose within a target range. At mealtimes, the user counts their carbohydrate intake and keys it into the pump, which then runs the algorithm to decide how much insulin is required and thus allowing the pump to deliver the dose. This is called an artificial pancreas or closed-loop system.
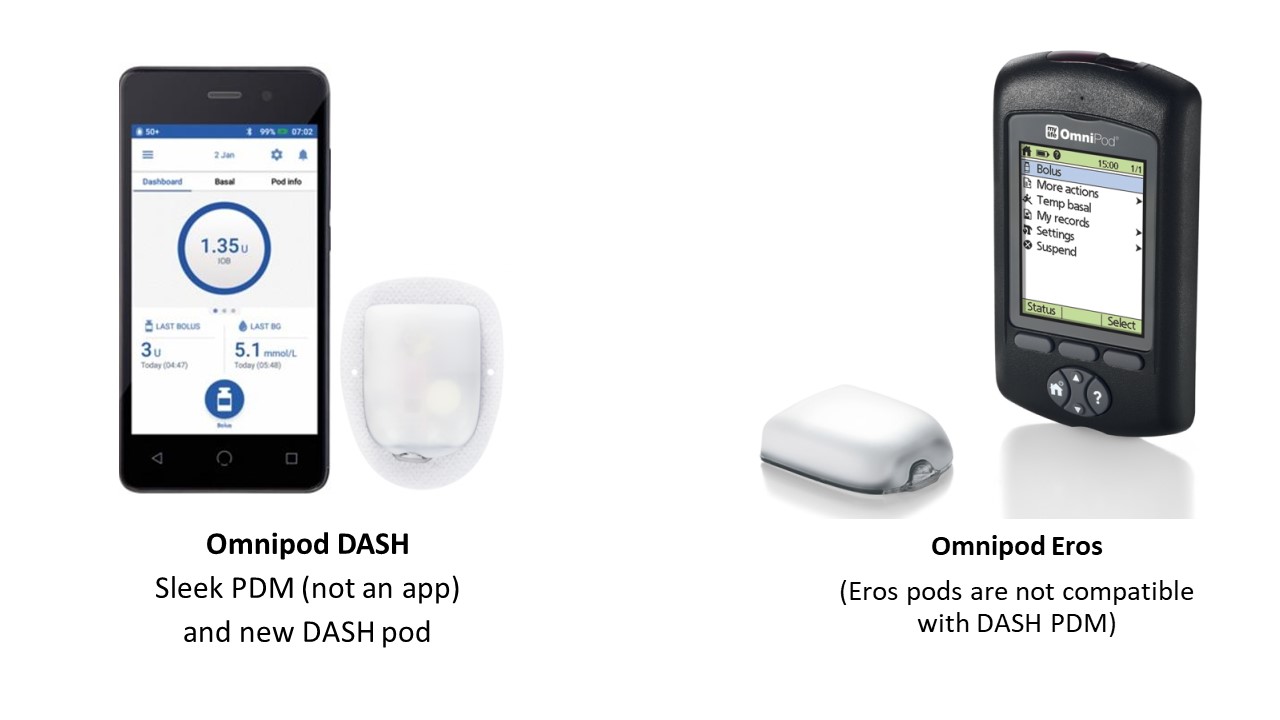
No. As of 2021, there is only one insulin pump system that is consider “tubeless” and is Omnipod (Insulet corporation). The pump reservoir and cannula are housed together in a single small device that can be worn in any part of your body. The device is also waterproof.
Pumps that have a “site” composed of a cannula and extension tubing for insulin administration include:
- T Slim (Tandem)
- MiniMed™ 770G and MiniMed™ 630G (Medtronic)


Diabeloop is a French company that has a hybrid close loop system approved to be used for type 1 diabetics. DBLG1 System, the AID (Automated Insulin Delivery) system from Diabeloop individualizes treatment by automating insulin decisions. It connects a CGM (Continuous Glucose Monitoring), an insulin pump and Diabeloop self-learning algorithm hosted in a dedicated handset to function as a hybrid-closed loop. The algorithm analyses data in real time and considers the physiology, history and data entries (meals or exercise) to determine either to maintain current settings, adjust or even stop basal insulin delivery to avoid a predicted low glucose level or deliver a bolus to correct a high glucose level.
Up until early 2021, it is only available in Europe.


How do I choose a pump?
There is NO perfect pump since all devices have benefits and drawbacks depending on your preferences. The table below summarizes our experience with several pumps common in the US.
Insulet OmniPod
- Tubeless, discreet, and relatively painless insertion
- Easy setup and pod changes
- Waterproof
- Wireless controller
- Lower upfront cost
- Must be thrown away every three days, or more frequently for people with high daily doses
- No integrated meter with OmniPod Dash
- Currently no Automated Insulin Delivery (close loop) availability
- Those who are highly active people
- Those who prefer a discrete pump without tubing
Medtronic MiniMed 670G System
- Hybrid closed-loop pump
- Auto Mode automatically adjusts basal-insulin based CGM readings
- Makes use of SmartGuard technology to stop insulin delivery for two hours if glucose levels reach a low
- Sensor must be calibrated 3-4 times per day
- Frequent system alerts are given while in Auto Mode
- The pump requires users to confirm mealtime and correct bolus recommendations
- People who struggle with nighttime hypoglycemia
- People who need help stabilizing glucose levels
Tandem t:slimX2
- Tubeless, discreet, and relatively painless insertion
- Easy setup and pod changes
- Waterproof
- Wireless controller
- Lower upfront cost
- Must be thrown away every three days, or more frequently for people with high daily doses
- No integrated meter with OmniPod Dash
- Currently no Automated Insulin Delivery (close loop) availability
- Those who are highly active people
- Those who prefer a discrete pump without tubing
A CGM works through a tiny sensor inserted under your skin, usually on your belly or arm. The sensor measures your interstitial glucose level, which is the glucose found in the fluid between the cells. The sensor tests glucose every few minutes. A transmitter wirelessly sends the information to a monitor.
The monitor may be part of an insulin pump or a separate device, which you might carry in a pocket or purse. Some CGMs send information directly to a smartphone or tablet.
A tiny CGM sensor under the skin checks glucose. A transmitter sends data to a receiver. The CGM receiver may be part of an insulin pump, as shown here, or a separate device.
CGMs are always on and recording glucose levels—whether you are showering, working, exercising, or sleeping. Many CGMs have special features that work with information from your glucose readings:
- An alarm can sound when your glucose level goes too low or too high.
- You can note your meals, physical activity, and medicines in a CGM device, too, alongside your glucose levels.
- You can download data to a computer or smart device to more easily see your glucose trends.
Some models can send information right away to a second person’s smartphone—perhaps a parent, partner, or caregiver. For example, if a child’s glucose drops dangerously low overnight, the CGM could be set to wake a parent in the next room.
- Twice a day, you may need to check the CGM itself. You will test a drop of blood on a standard glucose meter. The glucose reading should be similar on both devices.
- You will also need to replace the CGM sensor every 7 to 14 days, depending on the model.
- For safety it is important to act when a CGM alarm sounds about high or low blood glucose.
- You should follow your treatment plan to bring your glucose into the target range or get help.
Most people who use CGMs have type 1 Diabetes, but it is now approved (with certain insurance limitations) for diabetes type 2. CGMs are approved for use by adults and children with a doctor’s prescription. Some models may be used for children as young as age 2. Your doctor may suggest using a CGM system all the time or only for a few days to help adjust your diabetes care plan.
Compared with a standard blood glucose meter, using a CGM system can help you by:
- better managing your glucose levels every day.
- have fewer low blood glucose emergencies.
- need fewer finger sticks.
A graphic on the CGM screen shows whether your glucose is rising or dropping—and how quickly—so you can choose the best way to reach your target glucose level.
Over time, good management of glucose greatly helps people with diabetes stay healthy and prevent complications of the disease. People who gain the largest benefit from a CGM are those who use it every day or nearly every day.
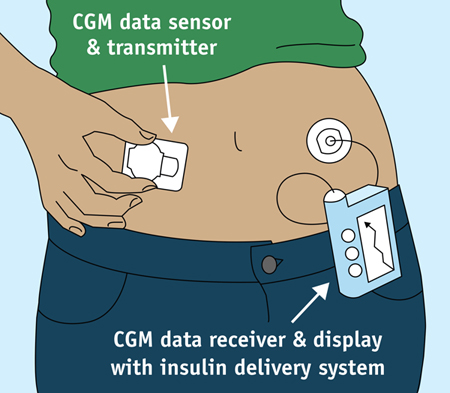
Photo courtesy: U.S. Food and Drug Administration
Need more information?
For more information about insulin pumps or continuous glucose sensor (CGM), please call Miami Diabetes and Endocrinology main office at (786) 433 2450 or schedule now.
Schedule an Appointment Today
& receive personalized treatment options.